Chelsea Yates
Diabetes is a chronic health condition that affects how the body converts food — particularly sugars — into energy, and identifying it early can make a critical difference in long-term health. UW Engineering researchers are rethinking how we detect and predict diabetes, bringing new tools closer to everyday life.

A professor of industrial and systems engineering, Shuai Huang has spent more than a decade studying type 1 diabetes risk. Photo: Mark Stone / University of Washington
Here, we highlight two projects: One research team is building new ways to model type 1 diabetes risk to better understand who is most likely to develop the disease. Another is creating a test strip for prediabetes designed to be simple, affordable and easy to use with a smartphone. Together, these efforts demonstrate how technology and data science are shaping a future where diabetes risk can be identified earlier — and managed more effectively.
Modeling the risk of type 1 diabetes
Type 1 diabetes (T1D) is a lifelong disease that happens when the body’s immune system attacks the cells that make insulin, a hormone that controls blood sugar. People with T1D need to take insulin every day to stay healthy. The condition often starts in childhood but can develop at any age. Researchers know that both genes and the environment play a role, but they’re still working to understand exactly what triggers it — and how to predict who will develop it.
That’s where Shuai Huang and his research partners come in. A professor of industrial and systems engineering (ISE) and data scientist who works at the intersection of health care, machine learning and engineering, Huang has spent more than a decade studying T1D risk.
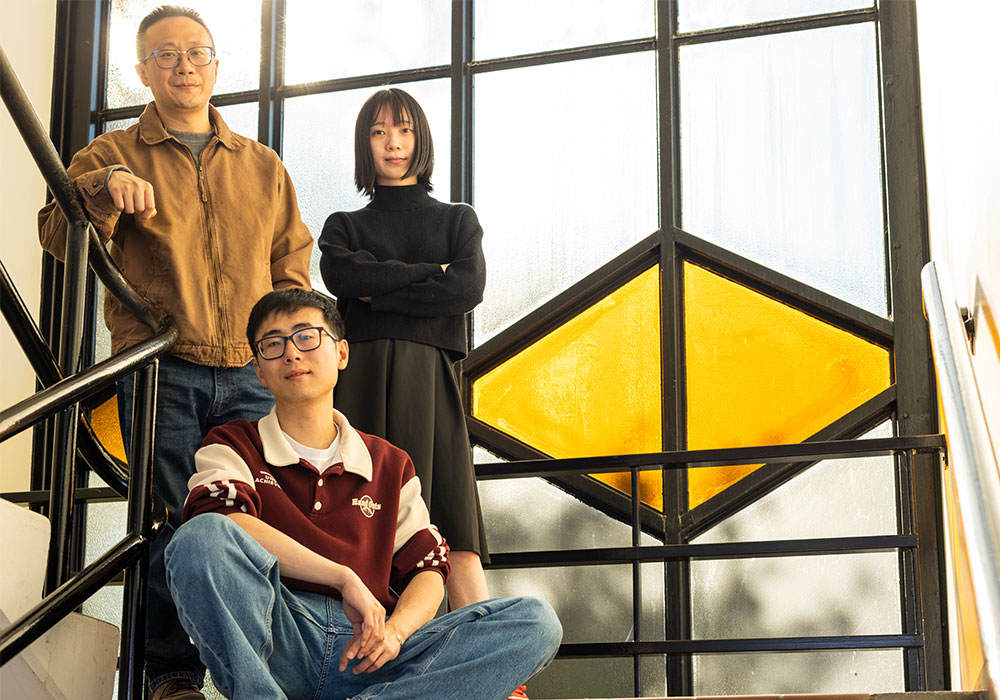
Huang, left, with ISE graduate students Congjing Zhang, right, and Ryan (Feng) Lin, center. Photo: Mark Stone / University of Washington
Today, Huang’s team is developing new frameworks for building more accurate, robust and responsive risk score models for T1D — tools that estimate how likely a person is to develop the disease based on their genes and environment. And while the models have improved greatly in recent years, a key problem remains: most are built on data from people of European descent. This means predictions can be less accurate for people from other backgrounds.
“Our goal is to make risk prediction representative of everyone,” Huang explains.
To do so, his group is creating an artificial intelligence pipeline that can detect imbalances in the data and learn both the shared and unique genetic patterns across populations. The team is also building an open-source repository so researchers worldwide can access and improve the models.
While genes offer important clues, they’re only part of the story. Something in the environment acts as the trigger for T1D — but what? For example, Huang says that rates of T1D are higher in the Pacific Northwest than many other parts of the U.S. One theory is that reduced sunlight, and therefore lower vitamin D levels, may play a role, since vitamin D helps regulate the immune system. “We can screen for genetic risk, but what we don’t know is what flips the switch,” says Huang. “AI and machine learning can help us search for hidden patterns.”
Huang partners with engineering and health experts at UW Medicine Diabetes, The Pacific Northwest Research Institute, Benaroya Research Institute, the University of South Florida and Texas A&M University, among others. Graduate students also play a key role: A team led by ISE Ph.D. student Ryan (Feng) Lin developed the Fair Collaborative Learning Model to help researchers evaluate disparities in datasets and improve prediction performance across groups with different data quality and size.
Another researcher in Huang’s lab, ISE Ph.D. student Congjing Zhang is designing digital twins — synthetic populations that let researchers test risk models under different scenarios. This could help avoid biased predictions that reflect only one region, such as the Pacific Northwest, or one ancestry group. The insights may also extend to other diseases, such as Alzheimer’s.
“The data is there,” Huang says. “The question is how to use it to make life better for patients.”

“Engineers can make a real impact in health care and medicine. We need people who can translate complex information into models and predictions that truly help patients.”
Smartphones for prediabetes screening
Type 2 diabetes occurs when the body can’t use insulin properly, causing blood sugar to rise over time. According to the U.S. Centers for Disease Control & Prevention, prediabetes — when blood sugar is higher than normal but not yet in the diabetes range — affects about one in three U.S. adults, and more than eight in ten don’t know they have it. Both conditions increase the risk of serious health problems, including heart disease, stroke and kidney failure. With early detection, however, people can make lifestyle changes that often delay type 2 diabetes, or even prevent it entirely.
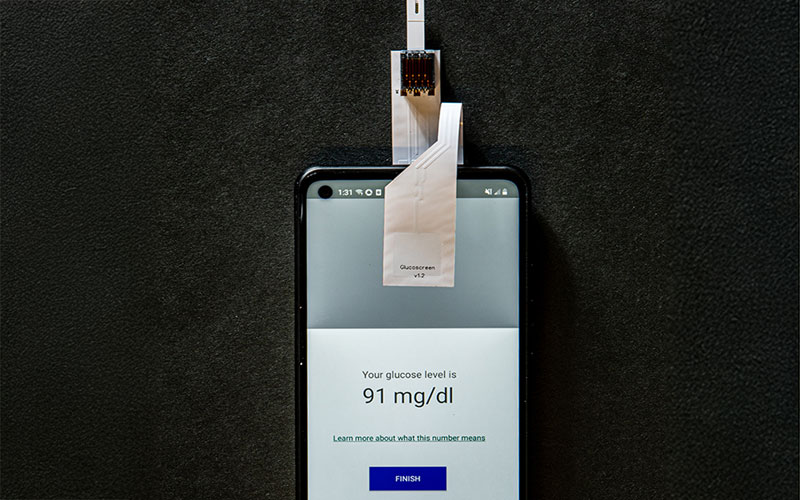


The GlucoScreen system turns a smartphone into a prediabetes screening tool using a modified test strip and low-cost circuitry that sends data through the touchscreen. Researchers are currently exploring ways to leverage additional built-in sensors and transmit data through audio signals. Photos: Raymond C. Smith / University of Washington
A few years ago, researchers in the UW’s Ubiquitous Computing Lab led by Shwetak Patel, a professor in the Paul G. Allen School of Computer Science & Engineering and of electrical and computer engineering, and UW Medicine introduced GlucoScreen, a system that turns a smartphone into a prediabetes screening tool. By pairing the electrochemistry of a standard blood glucose test strip with low-cost circuitry, GlucoScreen sent readings directly to a phone — no separate glucometer needed. In proof-of-concept studies conducted in lab and clinical settings, the system proved as accurate as conventional glucometers, demonstrating strong potential for low-cost, large-scale screening.

Allen School postdoctoral researcher Jason Hoffman
Now the team is focused on making GlucoScreen easier to use. Jason Hoffman (Ph.D. ’25), a postdoctoral researcher in the Allen School, is leading efforts to refine and simplify GlucoScreen for a broad range of users — from patients and clinicians to everyday individuals who want to manage their own health.
“Our original version was a modified test strip that drew power from the phone’s flash and transmitted data through the touchscreen,” explains Hoffman. “But phones have other built-in sensors found in nearly all devices, and we’re now exploring ways to leverage them, too.”
For example, the team is currently investigating how the standard placement of a phone’s USB-C port could enable new test strip designs, which could make test strips simpler for first-time users.
In conjunction, Hoffman is exploring creative ways to transmit test strip data through audio signals, keeping the system inexpensive and “plug-and-play” so it can work on nearly any smartphone without requiring special hardware modifications or attachments.
Future versions may go beyond detection. The team envisions a companion app that not only delivers results but also helps people manage their risk through lifestyle guidance and tracking. They’re also exploring how the technology could be applied to other health tests, such as cholesterol or hemoglobin A1C levels.
As part of UW CoMotion’s Postdoctoral Entrepreneurship Program this year, Hoffman is studying the commercial potential of GlucoScreen through usability testing and market research.
He’s motivated by the chance to improve health care access and empower people with personal information to manage their own health.
“Diabetes is a major and growing burden on individuals, families and health care systems,” he says. “Preventive care can make a huge difference, especially when risks can be identified early. GlucoScreen isn’t going to solve diabetes, but it could be a very helpful part of the solution.”
More engineering and health stories
Our faculty, staff and students are advancing health care, transforming research into real-world solutions for the public good.
Originally published November 10, 2025